Diagnostic update - Arcal Lick
Arcal Lick
ADC Newsletter April 2020: Acral Lick Granuloma Amy K.Shumaker (2019)
Article Overview
Acral lick dermatitis (ALD) is a complex problem. The disease can be complicated and multifactorial. Incessant licking due to pruritus, pain, compulsive behaviour or a combination of these can lead to secondary bacterial infections, which prevents or delays lesion resolution.
Take home Messages
ALD is multifactorial and can be frustrating to manage
ALD can affect dogs of any age, however large breed dogs are predisposed
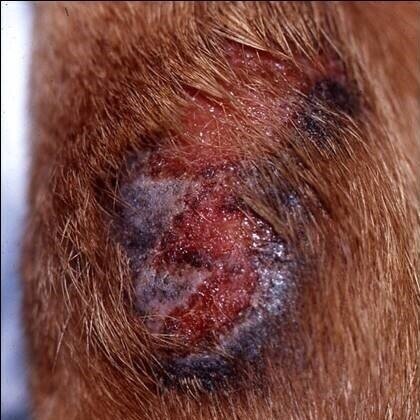
Clinically present as well circumscribed, raised, alopecic, erosive to ulcerated plaques affecting the distal extremities. Neoplasia must be ruled out.
A primary factor is the inciting cause.
Primary factors include pruritus from allergic disease (atopic dermatitis, cutaneous adverse food reaction, flea allergy dermatitis), previous trauma, foreign body, dermatophytosis, demodicosis, bacterial and Malassezia infections and hormonal disease or pain from joint disease or osteoarthritis, or neuropathy.
Primary psychogenic factors include obsessive compulsive disorders, anxiety, boredom, stress or attention seeking behaviour.
A perpetuating factor causes the desire to continue to lick the granuloma. These include secondary bacterial infections, keratin foreign bodies, osteomyelitis and learned or compulsive disorders.
A combination of diagnostic and treatment options are required to both resolve and prevent the recurrence of ALD
Before treatment
8 weeks after treatment
Pathogenesis and Clinical Presentation
Initially underlying erythema, scaling, crusting, alopecia and erosion results from frequent licking to one confined area. As the epidermis and dermis become exposed and traumatised, the sensory nerve fibres signal pruritus and this worsens the licking cycle. With chronicity, dermal fibrosis and epidermal hyperplasia result. This creates a plaque like appearance. Secondary bacterial infection manifests as folliculitis and furunculosis.
Diagnostic Investigation
A thorough dermatological exam will help determine whether there is evidence of an underlying allergic disease process. Cytological examination of direct impression smears and tape preparation samples are useful in identifying the presence of secondary bacterial and Malassezia organisms. Microbial culture and sensitivity tests are warranted in those cases that are refractory to first line antibiotics where there is partial or no response to treatment. Bacterial culture is also useful in guiding antibiotic choice. Deep tissue culture is preferred to superficial surface culture as there can be discrepancy in the bacteria isolated.
Skin scrapings, trichograms and fungal cultures can be used to diagnose ectoparasites and dermatophytes.
Orthopaedic examination including orthogonal radiographs of the affected area(s) should be performed to evaluate for underlying musculoskeletal disease such as osteoarthritis, osteomyelitis, periostitis and/or previous bony trauma.
In those cases where a neurological disorder is suspected, a neurological examination +/- EMG is recommended, especially for those patients with a history of previous trauma to the affected area.
Routine blood work, including a thyroid panel, as well as urinalysis can identify a potential endocrinopathy that may be the underlying trigger.
Neoplasia may be an underlying cause for chronic licking. Histopathology via incisional or excisional biopsy or cytological examination of a fine needle aspirate sample should be performed when a neoplastic process is suspected.
Behavioural disorders can be challenging to explore and diagnose in canine patients. Acral lick granulomas can manifest as stereotypical behaviour. This behaviour has previously been compared to human obsessive-compulsive disorders. It is important to consider whether stress may be playing a role ie. through the loss of a canine companion, separation anxiety, confinement throughout the day, lack of exercise or mental stimulation etc.
Treatment
It is imperative to successfully identify and address the primary and perpetuating factors in order to achieve lesion resolution and to control pruritus. Often, a combination of treatments are utilised.
Topical anti pruritic therapy
Physical barriers to prevent ongoing self-trauma include Elizabethan collars and bandages. Deterrent bitters sprays and creams may be useful in mild cases of pruritus. Topical and oral corticosteroids are effective in reducing both pruritus and inflammation. Fluocinolone and dimethyl sulfoxide (DMSO) is particularly effective as the DMSO increases the penetration of the fluocinolone through thickened tissue. Topical treatment should not be a replacement for systemic antimicrobial therapy.
Anti microbial therapy
Antimicrobial courses are often required for between 6-8 weeks, and often longer. This is due to deep tissue infection. As previously discussed, microbial culture and sensitivity testing is recommended.
Managing allergic disease
An elimination diet trial followed by dietary re-challenge remains the gold standard for diagnosing a cutaneous adverse food reaction. Once a food allergy is confirmed, the identified causative protein(s) is then avoided for life.
Allergen specific immunotherapy following intradermal and serology testing should be performed when atopic dermatitis is strongly suspected and only once other disease process have been ruled out. It is important to note that most acral lick dermatitis cases are chronic and it may take several months of anti pruritic and antimicrobial therapy before a diet trial or skin testing can be carried out. Where intradermal testing is not an option, oclacitinib, cyclosporin and/or systemic glucocorticoids may be used to control pruritus. Allergen specific immunotherapy is the preferred long term treatment due to the side effects of long term, high dose prednisolone usage.
Orthopaedic Disorders
A combination of surgery (where appropriate) and non steroidal anti inflammatory medications should be recommended when there is a musculoskeletal disorder involved.
Surgery
Surgical removal is difficult as acral lick granulomas commonly occur over flexural regions of distal extremities. Thus, wound dehiscence is a common post operative complication. Wound closure is not always possible because of the location.
C02 Laser Therapy
Laser therapy may be considered for acral lick granulomas that are non responsive to therapies discussed previously. Infection must be completely resolved prior to performing laser therapy or post operative complications will result, as well as poor outcome. Laser therapy can seal nerve endings, thus reducing the sensation of pruritus within the affected area.
Cryosurgery
There are no published articles in the literature on the use of cryotherapy in treating acral lick granulomas. The appeal for this technique is that it is much less invasive that surgical excision. One disadvantage is that multiple cryotherapy treatments are likely to be required.
Radiation
Radiation therapy is used to destroy nerve endings which breaks the itch-lick cycle. It should be noted that this treatment method does not treat the underlying trigger of pruritus but is more a symptomatic treatment.
Acupuncture
Evidence for the efficacy of canine acupuncture in alleviating pruritus is based predominantly from human medicine. There is some support for the use of acupuncture for acral lick granulomas, however as with radiation therapy, the underlying cause is not addressed. Adjunctive treatments are normally required.
Behavioural/Psychogenic
The management of behavioural disorders is multi modal and complex. Treatment must be ongoing or the undesirable behaviour (licking) will return. Environmental alteration to include more mental and physical stimulation is imperative. This may include puzzle like feeding toys and increasing the frequency of walks.
Selective serotonin re-uptake inhibitors (SSRI’s) are highly effective for managing the clinical signs of acral lick granulomas and preventing their recurrence. Fluoxetine is the most commonly prescribed SSRI for canine patients needing long term drug therapy. Clomipramine, a tricyclic antidepressant is also highly effective. Fluoxetine is preferred due to it having less adverse side effects compared to clomipramine.
Is your pet itchy, scratchy and distressed?
To make an appointment, call your local clinic or book online.
Murdoch Clinic
Murdoch Drive, Perth, WA 6150
Phone: +61 8 9360 7387
Email: dermnurses@murdoch.edu.au
Vet24
59 Erindale Rd, Balcatta WA 6021
Phone: +61 447 305 528
Email: animaldermatologyclinicperth@gmail.com
Animalius
6 Focal Way, Bayswater, Western Australia, 6053 Phone: +61 8 6166 3770
Email: dermatology@animalius.vet